INFORMATION SHEET FOR LAPAROSCOPIC BARIATRIC SURGERY
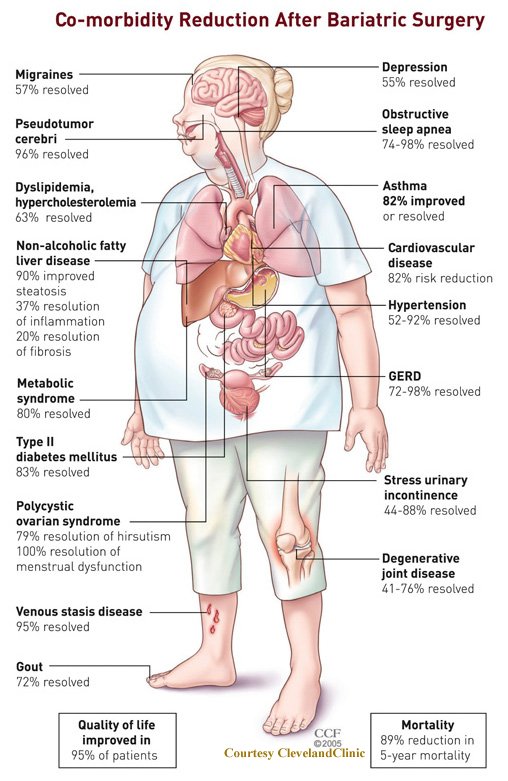
Comorbidities associated with Obesity.
Indications for Bariatric Surgery
The following are the indications of Bariatric Surgery according to 2005 APBSG consensus meeting for Asian people to:
- Obese patients with BMI >37.5 kg/m2 (Morbid Obesity),
- Obese patients with BMI >32.5 kg/m2 (Severe Obesity) in presence of diabetes or two significant obesity related co-morbitidies,
- Patients unable to lose or maintain weight loss by dietary or medical measures and
- Patients > 18 years and < 65 years of age.
EATING HABITS AND EXERCISE
Imp: Please follow the diet chart as per duly given to you at the time of first appointment. It is important during the initial recovery period you take the appropriate amount of calories, protein and vitamins in order to avoid feeling ill, weak and possible losing some hair. Your goal is to burn fat, not muscle, so taking in protein to maintain muscle bulk is very important. Take full advantage of the early period of lack of appetite to get into the right eating and exercising habits. Patients who fail to develop good dietary habits are more likely to regain weight in the longer term. If you go back to high calorie foods such as chips, cookies, soft drinks and do not stay active, then even the best bypass will fail. Your bariatric procedure should be regarded as a tool to aid your weight loss. The importance of behavioural factors cannot be overemphasised. It is therefore very important that you participate in our Patient Support Group as much as possible and seek dietary and psychological assistance whenever it is recommended or whenever you feel that you are struggling to achieve your goals. Studies have shown that patients who participate in patient support groups, and have their surgery carried out in the multidisciplinary environment, achieve better results.
UNREALISTIC EXPECTATIONS
Initial weight loss with the laparoscopic gastric sleeve can be very rapid. This ongoing weight loss can be psychologically addictive but ultimately it will slow down after six to nine months so it is best that you are prepared for this event. As has been stated previously, the most rapid period of weight loss is in the first few months, so this is the period when we recommend you begin your exercise regime with the assistance of our physiotherapy protocol. As you lose weight your exercise capacity will increase, making you feel better and fitter. The best average result from a laparoscopic gastric sleeve is 65% excess body weight over an 18-month period. Bear in mind that the goal of surgery is to make you healthier and improve your life expectancy and decrease the problems suffered by obesity related diseases, it is not to get you down to your ideal weight. The more weight you have to start with, the more weight you will probably lose with surgery and our recommended dietary and exercise regime. Try not to get caught in the trap of comparing your weight loss with others.
PREGNANCY
If you are a woman you should avoid pregnancy in the first year postoperatively. Periods of rapid weight loss are not the right time to be trying to get pregnant or trying to maintain and existing pregnancy. Also bear in mind that as you lose weight your fertility will increase and you are more likely to become pregnant. Female bariatric surgery patients can and do get pregnant and with appropriate support from obstetricians, will have an uneventful pregnancy. Obviously it is important should you get pregnant, that you bring to your obstetricians attention as soon as possible the fact that you have had bariatric surgery.
SMOKING
Smoking is a serious problem for bariatric surgical patients. It increases your risk of pulmonary complication and blood clots regardless of the procedure you have performed. I strongly recommend that if you are a smoker, that you try and stop smoking prior to surgery. Even stopping smoking a week before surgery can be of benefit.
You will meet our Anesthetist prior to your chosen bariatric procedure. This is done to make sure, as best as possible, that you have an acceptable risk of anesthesia. Anesthetists may recommend further medical or cardiac investigations at that time. If this is the case your surgery will have to be postponed until these tests have been completed and evaluated by our anesthetists.
General risks which apply to all abdominal surgery include but are not limited to the anesthetic (greater in the morbidly obese), deep venous thrombosis (DVT), pulmonary embolism, death, infection, bleeding, pneumonia, heart attack, stroke, bowel obstruction, intra-abdominal abscess, damages to intra-abdominal organs, adhesions, wound infections and Incisional hernias.
BLEEDING
Though it is unusual to have significant bleeding (< 1%) but blood transfusions and rarely relaparoscopy may be needed in case of significant bleeding.
INFECTION
Any surgery carries a risk of infection. The most common types are wound infections, urinary infections and chest infections. More serious types are blood infections, abscess and peritonitis. Although fortunately rare, some of these infections can progress to death, even if the source of infection is corrected and appropriately treated.
CLOTS
Blood clots in the veins in the legs or pelvis (DVT) can migrate to the lung (pulmonary embolism – PE), which can be fatal (Cause Death). These can occur after any type of surgery, and the risk persists after surgery for up to three weeks. The risk of this type of complication after bariatric surgery is less than 1%. However as it is such a serious complication and can result in sudden death, we take a number of steps to try and minimize the risks. You will be given injections to thin the blood, may be given stockings to compress your legs and when you are asleep in the operating theatre, machines will be used to squeeze the blood from your legs. These machines continue to be used on the ward when you are in bed and we encourage you to get up and walk about the ward as soon as possible. The risk of DVT is about 1:200 and the risk of pulmonary embolism about 1:1000. If you are identified as being a high-risk candidate, we may discharge you home on blood thinning injections for longer period in an effort to minimize your risk.
CHEST PROBLEMS
Pulmonary complications such as pneumonia, aspiration and atelectasis (partial collapse of the base of the lungs) can occur after any type of surgery under general anesthesia. The risk of this complication can be reduced by stopping smoking, early mobilization after surgery and working with our physiotherapists with chest exercises and learning Incentive Spirometry before surgery and continuing after surgery.
INCISIONAL HERNIAS
Incisional hernias are common after open bariatric surgery but thankfully rare after laparoscopic bariatric surgery. The risk is approximately 1% and if they do occur they tend to be small and easily repaired at a later date.
SMALL BOWEL OBSTRUCTION
The small intestine can get blocked by twists around scar tissue (adhesion) inside the abdomen that can occur after surgery. The other less common cause of bowel obstruction is an internal hernia. These types of obstructions can occur at any time and can occur many years after surgery. The rate of bowel obstruction after a laparoscopic sleeve is very low. Most obstructions after laparoscopic surgery can be successfully repaired laparoscopically.
WOUND INFECTION
These can occur with any type of surgery and even in clean surgery they occur in up to 5% of cases. They may require antibiotics, opening and drainage of the wound with packing. These wounds are then allowed to heal over a longer period of time with dressings as an outpatient. Patients who smoke are at increased risk of wound infection.
DAMAGE TO SPLEEN OR OTHER ORGANS
The spleen lies close to the upper portion of the stomach and can be injured during surgery. Fortunately it is very rare to injure the spleen during laparoscopic surgery and the rate is under 1%. If this was to happen you may require conversion to an open procedure and removal of the spleen. This will be avoided wherever possible. Pancreatitis is a rare but reported complication as is liver injury. These rarely require any surgical intervention.
BOWEL INJURY
Rarely the intestines or stomach can be injured at the time of surgery. If this occurs and is recognized, it will be repaired laparoscopically and the operation may be aborted at that point and rescheduled for a later date. If bowel injury was not recognized at the time then there is a risk of developing life-threatening peritonitis requiring further surgery and probable admission to Intensive Care.
DEATH
The mortality rate in gastric sleeve is 1:500 and laparoscopic gastric bypasses carry higher risk. You should recognize that although we do everything possible to minimize the risk, it cannot be reduced to zero. By undertaking bariatric surgery you are exchanging your risk of decreased life expectancy from weight loss related illnesses, to a short term increase in your risk of death during and immediately after the operation. Although the procedure is carried out with keyhole surgery it is still major surgery and you and your family should realize that any complications of this procedure could result in death.
STAPLE LINE LEAK
The stomach is divided with a stapling device in sleeve gastrectomy leaving two rows of steel staples behind. If this staple line breaks down and leaks, there is a risk of peritonitis, infection or an abscess. The risk of a leak is less than 3% but should it occur, it will require further surgery and the placement of drains. It is likely you will require a period of time in Intensive Care and if the infection is not controlled, it can become life threatening.
STAPLE LINE BLEED
There is a risk of bleeding from the staple line. This is in the order of less than 1%. Should this happen it is usually managed without the need for a further operation (Blood transfusion only) and settles by itself. Occasionally it may be necessary to take you back to theatre for a further laparoscopic procedure to wash out any blood in your abdominal cavity.
IT IS MY POLICY THAT IF I AM UNHAPPY WITH YOUR POST OPERATIVE RECOVERY, I WILL TAKE YOU BACK TO THEATRE FOR A LAPAROSCOPY. THIS MAY MEAN THAT YOU HAVE A 2nd PROCEDURE, WHICH SHOWS NO ABNORMALITY. HOWEVER STUDIES HAVE SHOWN THAT EARLY INTERVENTION FOR COMPLICATIONS PRODUCES THE BEST OUTCOMES.
VITAMIN MINERAL DEFICIENCIES
As the laparoscopic sleeve gastrectomy does not involve any alteration in the normal gut anatomy there is no particular risk of vitamin or mineral deficiency as seen in the gastric bypasses. Vitamin D deficiency is common in overweight patients and it is common to be placed on multivitamins for this reason. For patients undergoing Gastric Bypasses will require multivitamin, calcium and Vitamin D supplementation life long.
HAIRLOSS
It is not uncommon to have some thinning or loss of hair in the first few months after bariatric surgery. This is mainly temporary and is related to inadequate protein intake.
HIATUS HERNIA
A hiatus hernia occurs when part of the stomach slips up through the diaphragm into the chest. It is very common in the obese patient and will probably have been noted at your Gastroscopy. At the time of your bariatric surgery your hiatus hernia may be repaired with simple sutures to the hiatus. Generally the symptoms associated with a hiatus hernia of heartburn and reflux responds best to weight loss rather than anti-reflux surgery.
FAILURE TO LOSE WEIGHT
It is possible to cheat the operation and not lose weight. The idea of bariatric surgery is to adopt healthy lifestyle and supplement your diet and exercise regimen and not replace them and if patient starts taking high energy liquids, alcohol and junk food they may regain weight.
LARGE FOLDS OF SKIN
This is always a possibility with significant weight loss. There is no reliable way to determine before surgery how much or any of this will occur in your case. Age, exercise, speed of weight loss, elasticity of skin all play a role. The patients need to wait for at least 1 year to see if they need additional body contouring surgery. Plastic surgery procedures are available to correct excess skin problems and you can be referred to an appropriate plastic surgeon.
CONVERSION
Although it is always the intention to complete these operations laparoscopically, it is occasionally necessary to convert to an open operation for safety reasons. Should this happen you will have a prolonged stay in hospital and have increased risks of complication such as wound infection and incisional hernias.